Complete Title:
Role of Lateral Extra-articular Tenodesis in Restraining Internal Tibial Rotation: In Vitro Biomechanical Assessment of Lateral Tissue Engagement
Authors:
Zahab S. Ahsan, MD, Erin E. Berube, MS, Brian J. Frondorf, MD, Ho Bin Kim, BS, Niv Marom, MD, Zaid A. Zayyad, MD, Thomas J. Fraychineaud, MD, Ronak M. Patel, MD, Thomas L. Wickiewicz, MD, Carl W. Imhauser, PhD imhauserc, Andrew D. Pearle, MD, and Danyal H. Nawabi, MD
Abstract:
Background:
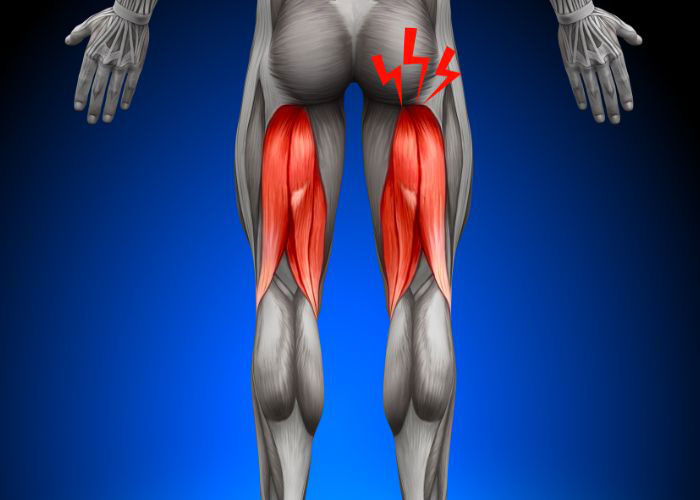
The way in which force increases in the anterolateral tissues and the lateral extra-articular tenodesis (LET) tissue to resist internal rotation (IR) of the tibia after anterior cruciate ligament (ACL) reconstruction in isolation and after LET augmentation, respectively, is not well understood.
Purpose:
(1) To compare in a cadaveric model how force increases (ie, engages) in the anterolateral tissues with IR of the tibia after isolated ACL reconstruction and in the LET tissue after augmentation of the ACL reconstruction with LET and (2) to determine whether IR of the tibia is related to engagement of the LET tissue.
Study Design:
Controlled laboratory study.
Methods:
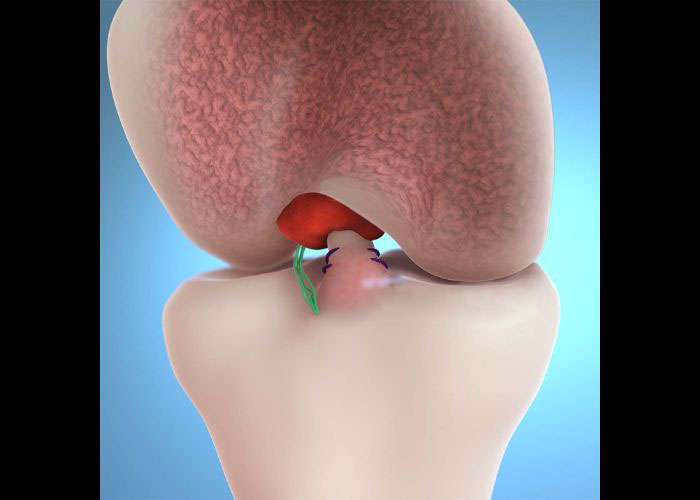
IR moments were applied to 9 human cadaveric knees at 0°, 30°, 60°, and 90° of flexion using a robotic manipulator. Each knee was tested in 2 states: (1) after isolated ACL reconstruction with intact anterolateral tissues and (2) after LET was performed using a modified Lemaire technique with the LET tissue fixed at 60° of flexion under 44 N of tension. Resultant forces carried by the anterolateral tissues and the LET tissue were determined via superposition. The way force increased in these tissues was characterized via parameters of tissue engagement, namely in situ slack, in situ stiffness, and tissue force at peak applied IR moment, and then compared (α < .05). IR was related to parameters of engagement of the LET tissue via simple linear regression (α < .05).
Results:
The LET tissue exhibited less in situ slack than the anterolateral tissues at 30°, 60°, and 90° of flexion (P≤ .04) and greater in situ stiffness at 30° and 90° of flexion (P≤ .043). The LET tissue carried greater force at the peak applied IR moment at 0° and 30° of flexion (P≤ .01). IR was related to the in situ slack of the LET tissue (R2≥ 0.88; P≤ .0003).
Conclusion:
LET increased restraint to IR of the tibia compared with the anterolateral tissue, particularly at 30°, 60°, and 90° of flexion. IR of the tibia was positively associated with in situ slack of the LET tissue.
Clinical Relevance:
Fixing the LET at 60° of flexion still provided IR restraint in the more functionally relevant flexion angle of 30°. Surgeons should pay close attention to the angle of internal and/or external tibial rotation when fixing the LET tissue intraoperatively because this surgical parameter is related to in situ slack of the LET tissue and, therefore, the amount of IR of the tibia.