Schedule an Appointment with a Dislocated Shoulder Specialist
If you believe you are suffering from an acute shoulder dislocation requiring an urgent appointment, we will do our best to provide a same-day or next business day appointment.

Individuals that have experienced a shoulder dislocation often experience shoulder instability. If you participate in high-contact sports or sports that involve repetitive overhead motion, you may be at an increased risk of shoulder dislocation. Board certified complex shoulder specialist, Doctor Ronak Mukesh Patel, has helped to diagnose and create specialized treatment plans for patients in Houston, Sugar Land, and Pearland, TX who have experienced shoulder dislocation. Contact Dr. Patel’s team today!
What is a dislocated shoulder?
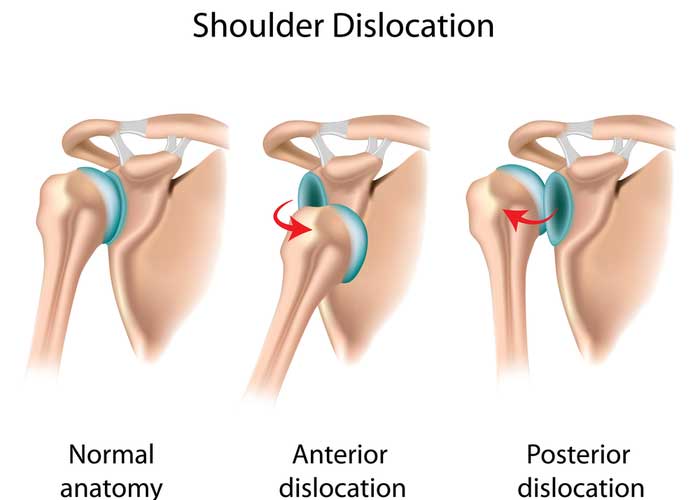
One of the three main shoulder joints is called the glenohumeral joint. This joint is found at the articulation of the head of the humerus (upper arm bone) into the glenoid socket of the scapula (shoulder blade). The glenohumeral joint boasts an incredible range of motion due to the ball-and-socket configuration of this joint. However, the muscles and ligaments surrounding this shoulder joint do not provide adequate stability with shoulder movement. This lack of stability can cause the shoulder joint to be easily separated in three different ways: backward, forward, or downward. Athletes that participate in aggressive contact sports, such as hockey, rugby, basketball, lacrosse and football, are more susceptible to suffering a shoulder dislocation. In the event a shoulder dislocation is presumed, immediate medical attention is essential. Dr. Ronak Mukesh Patel, orthopedic shoulder specialist serving patients in Sugar Land, Pearland, and the Houston, Texas area, has the knowledge and understanding, as well as substantial experience, in treating patients with a dislocated shoulder.
What causes shoulder instability?
The ligaments surrounding the shoulder joint can occasionally sustain a tear with a shoulder dislocation. When a ligament sustains a tear and does not heal properly, the ability to provide stability to the shoulder joint weakens, resulting in shoulder instability and increases the likelihood of recurrent shoulder separations. Repetitive overhead motions seen in sports like swimming, volleyball, tennis, baseball, and cricket can make the athletes that participate in these sports more susceptible to shoulder instability.
What are the symptoms of a dislocated shoulder?
The most common complaint of a shoulder dislocation is sharp shoulder pain immediately following an injury. Other common symptoms of a dislocated shoulder, or shoulder instability, can include:
- An obvious visual deformity of the displaced shoulder
- Pain and/or swelling
- Numbness of the affected arm
- Decreased range of motion
- Difficulty with arm movement
- A “popping” or “crunching” sensation
How is shoulder instability diagnosed?
A detailed medical history will be obtained by Dr. Patel to include the precipitating injury and any other prior shoulder conditions. A comprehensive physical examination will then be conducted to differentiate between a shoulder dislocation or shoulder instability. X-rays and magnetic resonance imaging (MRI) may be performed depending on the injury severity. Dr. Patel may also request an arthrogram, a diagnostic imaging technique using dye injected into the shoulder joint to identify any damage.
What is the treatment for a shoulder dislocation or shoulder instability?
If there is suspicion of a shoulder dislocation, immediate medical care by a medical professional or an orthopedic shoulder specialist is highly encouraged.
Non-surgical treatment:
When a shoulder separation is confirmed by imaging or physical examination, the reduction of the shoulder joint is of primary concern. The manual manipulation of the humeral head back into the glenoid socket should only be performed by a professional that is proficient in performing this reduction technique. Upon a successful shoulder reduction, the shoulder pain should be considerably diminished almost immediately.
A sling will then be applied to immobilize the shoulder joint allowing the ligaments to heal properly. Pain and inflammation can be further reduced with a combination of rest, ice application, and non-steroidal anti-inflammatory medications (NSAIDs). If the pain and swelling persist with oral medications, a corticosteroid injection can be administered directly into the glenohumeral joint. A physical rehabilitation program will be designed to strengthen the shoulder muscles and restore range of motion to the shoulder.
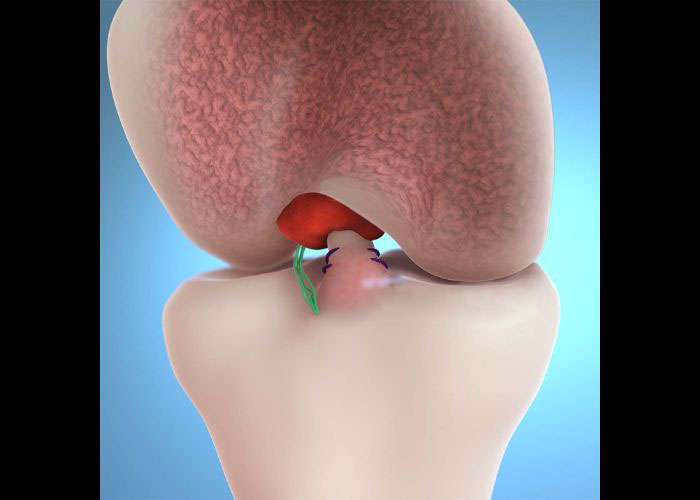
Surgical treatment:
For patients with severe or chronic shoulder instability, or in the event of a failed shoulder joint reduction, a shoulder arthroscopy may be recommended by Dr. Patel. This minimally invasive surgical method involves a small camera (arthroscope) and specialized surgical instruments to visualize and repair the damaged shoulder ligaments. This arthroscopic repair technique is effective for correcting shoulder instability while also shortening the recovery period for patients to return to their normal daily activities. He also has extensive experience in performing open stabilization procedures to treat shoulder instability in selected patients. Dr. Patel believes in individualizing treatment based on the injury, exam and imaging finds, patient factors, and goals.