OATS Surgeon

Patients who have a small area of cartilage and bone damage in the knee due to wear and tear or from an injury may qualify for an OATS procedure. Osteochondral Autograft Transfer has a high success rate if patients follow physical therapy protocols. Doctor Ronak Mukesh Patel, provides diagnosis and both surgical and nonsurgical treatment options for patients in Sugar Land, Pearland, and the Houston, Texas area who have a small area of articular cartilage damage in the knee. Contact Dr. Patel’s team today!
What is OATS or an Osteochondral Autograft Transfer in the knee?
The knee joint is lined with a smooth, slippery surface called cartilage. Found at the end of the bones, articular cartilage helps joints glide smoothly and without pain. It gives the knee flexibility. Sports activities, or wear and tear from aging can cause the cartilage to break down and become damaged. The result can cause pain, stiffness and swelling of the knee joint. An osteochondral autograft transfer, commonly known as the OATS procedure is a proven treatment that brings long-term pain relief to patients with damaged articular cartilage obtained from the patient’s own knee. The autograft is obtained from an area of the knee where the cartilage is either not needed or a non-weight bearing area so that it does not cause secondary pain or issues. Dr. Ronak Mukesh Patel, orthopedic knee surgeon has the experience and expertise to successfully perform the OATS procedure for qualifying patients in Sugar Land, Pearland, and the Houston, Texas area.
What is the difference between an Autograft Transfer and an Allograft Transplant?
Essentially, they are used to replace damaged cartilage and bone in the knee using healthy cartilage and bone from a separate source. The difference between the two is the source of the donor cartilage and bone. An autograft obtains the cartilage from the patient’s own knee, whereas an allograft means tissue is obtained from a donor or tissue bank. The OATS procedure is an osteochondral autograft obtained from the patient’s own knee.
How is OATS done?
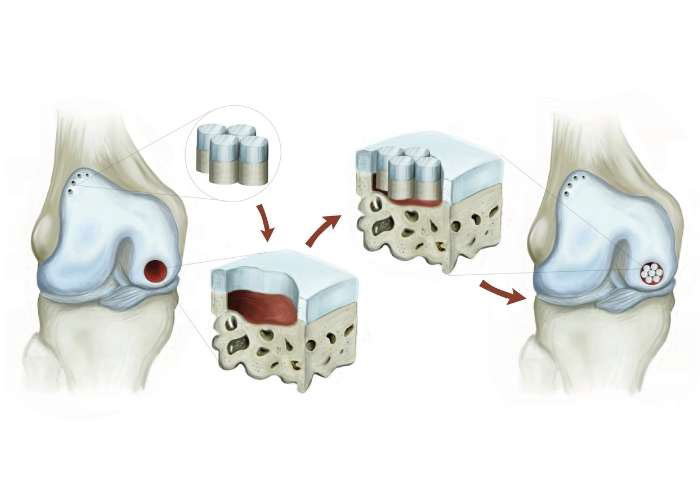
The OATS procedure is done in four steps:
- Patel will first inspect the knee arthroscopically to find the exact area and size of damage.
- An open incision is made in the correct area of the knee and the damaged cartilage is prepared by using a coring tool to make perfectly round holes where the damage is found. The small hole or holes are sized to fit the replacement “plug”.
- A small plug of normal bone and cartilage is harvested from the patient’s knee in a non-weight bearing area.
- The plug is then placed in the area that was prepared and fits tightly. Over time, the implanted bone and cartilage will incorporate into the new area and will heal the previous damage.
Why would I need a cartilage transfer?
Patients with cartilage injuries result from sports, falls, accidents, or wear and tear. Since articular cartilage cannot heal on its own, joint pain, inflammation, and trouble moving can occur. Osteochondral autograft transfer, or OATS, is ideal for patients with small areas of cartilage damage that can be easily repaired with a graft. Wear-and-tear types of arthritis, called osteoarthritis, is a degenerative condition so most patients with large or diffuse areas of cartilage loss are not candidates.
What is the advantage of OATS versus Osteochondral Allograft (OCA)?
OATS is the preferred technique compared to OCA as the patient’s own cartilage and bone is more reliable than when the cartilage is replaced from a donor (OCA). However, in some cases OATS may need be possible such as when the area of cartilage damage is too large.
What is the recovery time after an OATS procedure?
Patients who are appropriately selected to undergo an OATS procedure have a high success rate of cartilage restoration. Patients who undergo OATS surgery can expect the following:
- Non-weight bearing on the joint for approximately 4-6 weeks.
- Immediate range of motion in the knee with physical therapy starting the day after surgery.
- After 4-6 weeks, patients may begin to put weight on the joint as tolerated.
- Specialized and patient-specific physical therapy is required and is designed to strengthen the surrounding joint muscles and keep the knee mobile.
- Return to reports and full activity is around 5 to 6 months.