What is a patella dislocation?
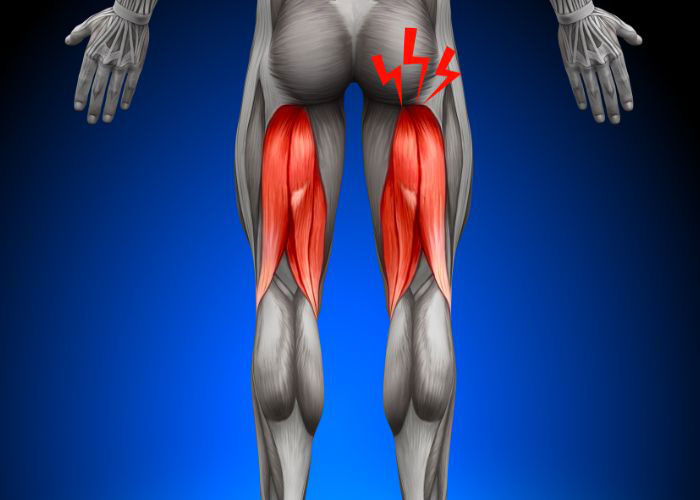
The knee joint is formed by the articulation of the patella (kneecap) with the femur (thigh bone) and tibia (shin bone). The patella is anchored in place by the quadriceps tendon, attached to the femur, and the patellar tendon, attached to the tibia. By strengthening the quadriceps tendon on the femur, the patella is important for knee extension. The undersurface of this sesamoid bone is lined with a slippery white articular cartilage allowing seamless movement of the patella along the trochlear groove. In the event of a traumatic blow directly to the knee or abnormal twisting motion, the patella can be forced out of the trochlear groove causing a patella dislocation. The structures of nearby ligaments and tendons can be compromised and weakened from the kneecap dislocation which in turn increases the risk of subsequent patellar dislocations. Severe dislocations can result in more extensive and complex damage to the surrounding soft-tissue structures. Dr. Ronak Mukesh Patel, orthopedic knee specialist serving patients in Sugar Land, Pearland, and the Houston, Texas area, has the knowledge and understanding as well as substantial experience in treating patients who have experienced a patella dislocation.

What are the symptoms of a patella dislocation?
The body frequently responds to a patella dislocation with severe knee pain and rapid inflammation in hopes of returning the kneecap to its correct anatomical position. Other common symptoms of a patellar dislocation can include:
- An obvious visual deformity of the knee
- A “catching” or “locking” sensation
- Knee instability or the feeling that the knee will “give way”
- Pain of the inner ligaments that continues after patellar relocation
- Hearing an audible “pop” at the time of injury
How is a patella dislocation diagnosed?
A comprehensive medical history will be collected by Dr. Patel to include the initial injury, any prior patellar dislocations, or other previous knee conditions. This will be followed by a thorough physical examination to assess ligament laxity. Diagnostic imaging tools, such as x-rays and magnetic resonance imaging (MRI), may be requested by Dr. Patel. X-rays can determine if any other bone-related injuries, such as a fracture, occurred as a result of the patella dislocation. An MRI can identify damage to the other soft-tissue structures within the knee joint and any other anatomical abnormalities such as bone spurs or loose bodies.
What is the treatment for a patella dislocation?
It is strongly encouraged to seek medical attention by an orthopedic knee specialist, or another medical professional, in a timely manner if a patella dislocation is suspected.
Non-surgical treatment:
A joint reduction technique will be performed in the event that the patella does not spontaneously return to its normal position after being dislocated. This technique should only be performed by a medical professional who is experienced in the manual manipulation of the patella back into the trochlear groove.
Non-surgical therapies alone are often successful for patients that sustained mild ligament injuries from a patella dislocation. A knee brace is applied after a successful patellar reduction to stabilize and protect the surrounding knee joint structures during the healing process. A combination of RICE (rest, ice, compression, elevation) and non-steroidal anti-inflammatory medications (NSAIDs) is recommended for pain and inflammation management. When appropriate, a physical rehabilitation program may be prescribed by Dr. Patel to restore mobility and strength to the knee joint.
Surgical treatment:
In the event of failed conservative or non-surgical therapy, damage to multiple knee joint structures, or other extensive or complex knee injuries, surgical intervention may be necessary to restore the function of the knee joint. Because of the greater likelihood of future patella dislocations due to the disruption in ligament structure, Dr. Patel may implement one or more of the following surgical procedures to restabilize the patella and return patients to their normal daily activities.
- Lateral Retinaculum Release: The most common surgical treatment for patellar instability involves the release of the lateral retinaculum, a fibrous tissue found on the outer patella, to alleviate tension on the outer knee and helps to realign the kneecap.
- A new groove for the patella is created by reshaping the distal femur. This technique is typically reserved for patients with severe patellar instability.
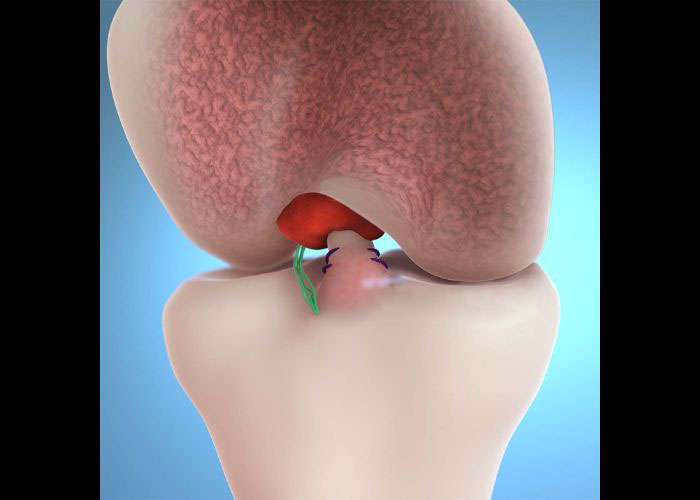
- MPFL Reconstruction: The damaged portions of the medial patellofemoral ligament (MPFL) are excised and removed, and the remaining tissue is sutured back together. If there is not enough tissue remaining, a tissue graft, either from the patient (autograft) or donor tissue (allograft), can be implemented to provide a new surface for new tissue to grow.
- Medial Imbrication: This minimally invasive procedure, also known as reefing, tightens the tissues of the inner knee.
- Tibial Tubercle Osteotomy: This technique is performed for patients that experience a patella dislocation due to a shallow trochlear groove. To correct for this abnormal lower extremity alignment, the tibial tubercle (bony prominence of the shin bone) is shifted, with the patellar tendon still attached, to another position on the tibia often resulting in the patella being pulled inward.
Patella Dislocation Specialist

Are you an athlete who participates in sports that requires rapid changes of direction like soccer, MMA, Lacrosse, hokey or football? If so, you may be at risk of suffering a patella (kneecap) dislocation. Symptoms of a kneecap dislocation are rapid, acute swelling and severe knee pain until the kneecap is relocated to its original position. Kneecap dislocation specialist, Doctor Ronak Mukesh Patel, provides diagnosis as well as surgical and nonsurgical treatment options for patients in Houston, Sugar Land, and Pearland, TX who have suffered a patella dislocation. Contact Dr. Patel’s team today!