What is knee arthritis?
The knee joint is formed when the femur (thigh bone), tibia (shin bone), and patella (knee cap) join together. Each of these bones is surrounded by a layer of cartilage that enables painless joint movement while also protecting the bone. There are additional soft tissue structures, such as the meniscus and synovial membrane, that allow the knee joint to seamlessly function. However, these structures can become damaged and affect their capability to properly function. Any injury or damage to these soft-tissue structures can lead to chronic pain, inflammation, and stiffness which can eventually limit an individual’s ability to perform daily activities. Dr. Ronak Mukesh Patel, orthopedic knee specialist serving patients in Sugar Land, Pearland, and the Houston, Texas area, has the knowledge and understanding, as well as substantial experience, in treating patients who have experienced knee arthritis.
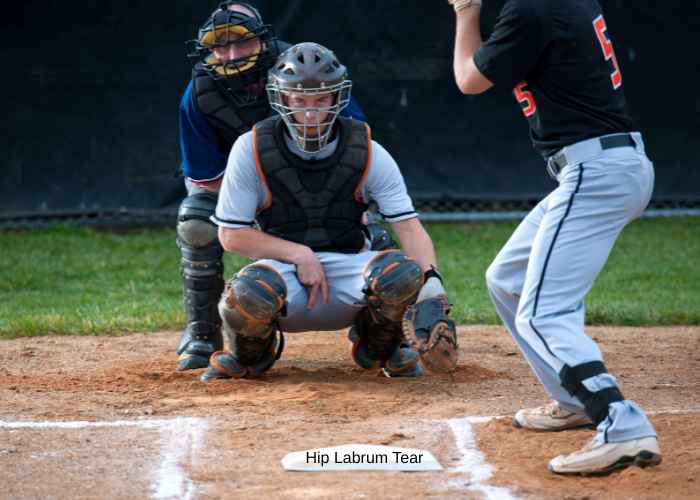
Are there different types of knee arthritis?
There are three different types of knee arthritis:
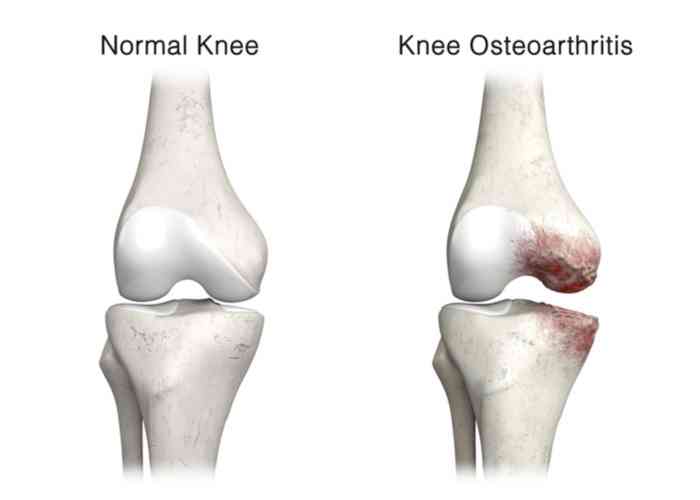
- Osteoarthritis: This is the most common type of knee arthritis and affects the articular cartilage in patients over the age of 50. The cartilage layer surrounding the ends of the bones naturally degenerates from the aging process. The excessive grinding of this fraying tissue against the other joint structures results in a gradual onset of knee pain and eventually leads to bone-on-bone movement. Bone spurs can also develop in this “wear and tear” form of knee arthritis.
- Rheumatoid Arthritis: This form of knee arthritis is an autoimmune condition that affects the synovial membrane and articular cartilage. These joint structures are attacked and destroyed by the body’s own immune system. The swelling of the synovial membrane causes knee pain and stiffness. Both knee joints are typically affected in this form of knee arthritis.
- Post-traumatic Arthritis: A knee injury, such as a bone fracture, that damages any joint structures can develop into arthritis, even years after the initial injury. Ligament injuries and meniscal tears can cause additional stress on the knee joint resulting in joint instability and the eventual onset of arthritis.
What are the symptoms of knee arthritis?
The most common symptom shared among all three types of knee arthritis is knee pain that slowly develops and becomes progressively worse over time. Inflammation of the affected knee is also frequently reported. Individuals often report knee pain is worse in the morning and can change with the weather. Some other common complaints of knee arthritis include:
- Knee stiffness
- Temporary worsening of knee pain after strenuous activity
- Difficulty with bending or straightening the affected knee
- A “buckling” sensation or weakness in the affected knee
- Increased knee pain and swelling after extended periods of resting or sitting
How is knee arthritis diagnosed?
The process of diagnosing knee arthritis begins with an interview to gather a comprehensive medical history. This will include any previous knee injuries or underlying health conditions that may contribute to knee arthritis. Following this interview, Dr. Patel will conduct a thorough physical examination to analyze for areas of pain and tenderness and any signs of damage to the surrounding muscles, ligaments, and tendons. This examination also evaluates the stability and range of motion of the knee joint and identifies any gait abnormalities or if other joints are also affected.
Knee arthritis can occasionally be difficult to diagnose as the available imaging techniques may not detect subtle changes of the knee cartilage. However, a combination of the patient’s medical history, physical examination, and diagnostic imaging studies, such as x-rays and magnetic resonance imaging (MRI), can provide a better understanding for determining the cause of knee pain.
What is the treatment for knee arthritis?
Dr. Patel will evaluate the patient’s age, activity level, medical history, and recovery goals with the specific form of arthritis to design an individualized treatment plan.
Non-surgical treatment:
Patients with mild forms of knee arthritis may respond well to non-operative therapy options. Lifestyle modifications, such as limiting strenuous activities and losing weight, can slow the progression of knee arthritis. A combination of RICE (rest, ice, compression, elevation) and non-steroidal anti-inflammatory medications (NSAIDs) can help minimize any pain and inflammation. Corticosteroid and viscosupplementation (hyaluronic acid) injections directly into the knee joint can also be administered if the pain persists with oral medications. Newer alternative therapies are also available such as biologic treatments with platelet-rich plasma (PRP) or the use of stem cells. When appropriate, Dr. Patel will design a physical therapy program that is specific to the patient’s needs.
Surgical treatment:
However, surgical intervention may be necessary for patients with more severe knee arthritis symptoms or those that did not respond well to initial non-operative therapies. There are several different surgical procedures available for the treatment of knee arthritis. Dr. Patel may perform or suggest one or more of the following techniques:
- Knee Arthroscopy: This minimally invasive surgical procedure involves a small camera (arthroscope) and specialized surgical instruments to resect any damaged tissue fragments. This technique is used to alleviate symptoms, but it does not prevent further arthritic damage to the knee joint. Arthroscopy is typically reserved for special cases of isolated cartilage defects, young patients with other addressable pathology, knee preservation procedures, etc. and is not the mainstay of treatment for osteoarthritis.
- Synovectomy: The synovial membrane is removed to reduce joint pain and swelling. This procedure is reserved for patients with damage to this joint lining from rheumatoid arthritis.
- Cartilage Grafting: Healthy cartilage tissue is harvested from the patient or donor and inserted to fill any voids in the native articular cartilage. Younger patients with small cartilage defects are ideal candidates for this technique.
- Osteotomy: A wedge is cut and removed from the end of the femur or tibia closest to the knee joint. This surgical technique is performed when one side of the knee joint is damaged and the patient exhibits signs of early-onset osteoarthritis. By reshaping these bones, the weight is shifted away from the damaged side of the joint to reduce pain and substantially improve knee function.
- Partial or Total Knee Replacement: Also known as knee arthroplasty, this procedure replaces the damaged bone and cartilage with metal and plastic joint surfaces to restore knee function. This surgery is reserved for patients with advanced knee arthritis that have exhausted all other treatment options.
Knee Arthritis Specialist

Are you suffering from knee pain, stiffness and sometimes popping or cracking in the knee? If so, you may have osteoarthritis of the knee. Knee osteoarthritis specialist, Doctor Ronak Mukesh Patel, provides diagnosis as well as surgical and nonsurgical treatment options for patients in Houston, Sugar Land, and Pearland, TX who are experiencing knee pain caused by osteoarthritis. Contact Dr. Patel’s team today!